View our Product Catalog to find products you can try for free.
 menu
menu
-
0
Basket
- WHERE TO FIND US
-
US - English
Latin America
Europe
- Belgique - français
- België - Nederlands
- Danmark - Dansk
- Deutschland - Deutsch
- España - Español
- Finland - svenska
- France - Français
- Ireland - English
- Italia - Italiano
- Lietuva - Lietuvių
- Nederland - Nederlands
- Norge - Norsk
- Schweiz - Deutsch
- Suisse - français
- Suomi - suomi
- Sverige - svenska
- Svizzera - Italiano
- UK - English
- Österreich - Deutsch
Asia/Pacific
- Sign up or Login
-
Products
New Product
New Image Soft Convex CeraPlus skin barrier with a unique combination of fit and formulation.
Try It Free -
Ostomy Care
- CeraPlus™ Line of Products* A guide to our lines of products that meet your needs for security and skin health
- Security and Skin Health CeraPlus™ Products help keep healthy skin healthy
- Testimonials Hear from users of our CeraPlus™ Products
- Ostomy Care Learning Center Education, resources, and quick tools
- Clinical Education Resources that include research findings and learning opportunities for healthcare professionals
- Quick Educational Tools Helpful PDFs and videos for before and after ostomy surgery, including international resources
CeraPlus™ Product Selector
Selecting the Right Ostomy Product Can Make All the Difference
Learn More -
Continence Care
- Discover our Continence Care Products Our range of intermittent catheters has something for everyone who self-catheterizes, whatever their condition
- UTI Prevention Videos and articles about how to avoid urinary tract infections and improve your quality of life
- Learning Center Resources to help you learn more about bladder health, intermittent catheterization, and living life with a neurological condition
- Quick Educational Tools Helpful PDFs and videos to increase your continence care knowledge
- Clinical Education Educational resources for Healthcare Professionals
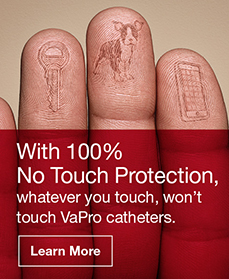
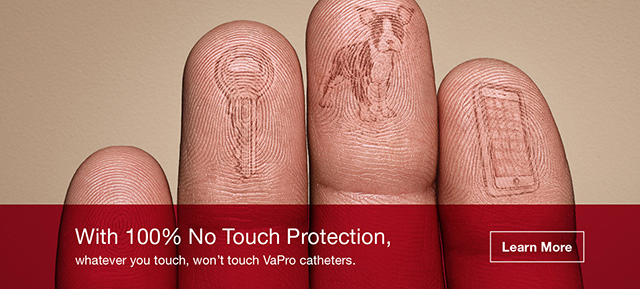
VaPro™ Intermittent Catheters
With 100% No Touch Protection, whatever you touch won't touch VaPro™ catheters
Learn More -
CRITICAL CARE
- SECURE START SERVICES
-
About
- Career Opportunities Share our legacy and help shape the future
- Associate Stories Learn what it is like to be a Hollister Associate
- Environmental Policy Learn more about our commitment to being good stewards of the environment.
- Global Locations Manufacturing and distribution centers and offices around the world
- Hollister History Built on the legacy of our founder
- News and Events News and Events
- SELECT COUNTRY
- Contact Us
- Where to Buy
Intermittent Catheter Reimbursement in the U.S.
The ever-changing healthcare landscape may raise many questions around reimbursement and coverage of intermittent catheters. But we'd like to make it a little simpler.
Onli™ Intermittent Catheter
- Code A4351 reimbursement
- Prehydrated and ready to use with pure water vapor hydration technology
- Ergonomic gripper on 16" catheter
- Easy open package
VaPro Touch Free Hydrophilic Intermittent Catheter
- Code A4353 reimbursement
- Coudé available under Code A4352
- Prehydrated and ready to use with pure water vapor hydration technology
- Protective tip and sleeve
- Integrated collection bag with handle
Coding Guidelines and Coverage Guidance
-
Code A4351 Coding Guidelines and Coverage Guidance
An A4351 catheter is an intermittent urinary catheter, with a straight tip, and with or without coating (Teflon, silicone, silicone elastomeric, or hydrophilic).
Intermittent catheters are covered to drain urine from the bladder for a patient who has permanent urinary retention. Permanent urinary retention is defined as when a patient is not expected to be medically or surgically cured within three months. For each catheterization episode, Medicare will cover one catheter (A4351 or A4352) and an individual packet of lubrication (A4332).
Patients can get up to 200 intermittent catheters each month.
For the full and most up-to-date policy, please visit www.cms.gov and search "L33803".
-
Code A4352 Coding Guidelines and Coverage Guidance
An A4352 catheter is an intermittent urinary catheter, with a coudé (curved) tip, and with or without coating (Teflon, silicone, silicone elastomeric, or hydrophilic).
Intermittent catheters are covered to drain urine from the bladder for a patient who has permanent urinary retention. Permanent urinary retention is defined as when a patient is not expected to be medically or surgically cured within three months. For each catheterization episode, Medicare will cover one catheter (A4351 or A4352) and an individual packe of lubrication (A4332).
A coudé tip catheter for females is rarely needed and justified. When a coudé tip catheter is prescribed, medical necessity must be documented in the medical record. An example would be the inability to catheterize with a straight tip catheter.
Patients can get up to 200 intermittent catheters each month.
For the full and most up-to-date policy, please visit www.cms.gov and search "L33803".
-
Code A4353 Coding Guidelines and Coverage Guidance
An A4353 catheter is an intermittent urinary catheter with insertion supplies (kit), which includes a catheter and all supplies necessary for a single, sterile insertion.
Intermittent catheterization using a sterile intermittent catheter kit (A4353) is covered when a patient requires catheterization and meets one of the following criteria:
- Lives in a nursing facility
- Is immunosuppressed
- Has vesico-ureteral reflux
- Is a pregnant spinal cord injured female with neurogenic bladder
- Has had two or more urinary tract infections (UTI) during a 12-month period while using sterile intermittent catheterization with A4351/A4352 and sterile lubricant A4332
A patient would be considered to have a urinary tract infection if they have a urine culture with greater than 10,000 colony forming units of a urinary pathogen AND concurrent presence of one or more of the following signs, symptoms or laboratory findings:
- Fever (oral temperature greater than 38º C [100.4º F])
- Systemic leukocytosis
- Change in urinary urgency, frequency, or incontinence
- Appearance of new or increase in autonomic dysreflexia (sweating, bradycardia, blood pressure elevation)
- Physical signs of prostatitis, epididymitis, orchitis
- Increased muscle spasms
- Pyuria (greater than 5 white blood cells [WBCs] per high-powered field)
Patients can get up to 200 intermittent catheters each month.
For the full and most up-to-date policy, please visit www.cms.gov and search “L33803”.
Still have questions on reimbursement?
Hollister Secure Start services can provide answers for you and your patients.
Feel free to give us a call at 1.800.808.7456.
Hollister Secure Start services are unique and designed to support people as they live their lives with ostomy or bladder management issues. These services are free of charge, and there is no obligation to purchase anything to receive them. Product samples are provided for the patient’s trial use and cannot be resold or billed. There is no obligation to accept samples or participate in insurance-matching to identify supplier options. Hollister reserves the right to change Hollister Secure Start services at any time.
The reimbursement information provided herein is intended to provide general information concerning coding of Hollister products only. Hollister does not guarantee coverage or payment for any product. The ultimate responsibility for proper coding, satisfying reimbursement requirements, and obtaining reimbursement remains with the provider. Coding and coverage policies and guidelines are complex, can vary from one carrier or region to another, and are updated frequently. Providers should check with their local carriers or intermediaries often and should consult with counsel, a reimbursement specialist, and/or DMECS website for any coding, coverage, reimbursement, or billing questions.
Quick Links and Resources
-
Skin Health Alliance Accreditation for Ostomy Products
-
Stoma Advocate Makes History Swimming Across the English Channel
Gill Castle becomes the first person with a stoma to make the swim alone.
Read More -
Customer Profile: Rachel Stokes
Rachel Stokes, a Hollister ostomy consumer, shares her ostomy journey.
Read More -
Hollister Incorporated Releases Second Annual Sustainability Report
The 2022 Sustainability Report communicates Hollister‘s progress under the pillars of Environment, S...
Read More -
Hollister Incorporated Expands Operations in Lithuania
Manufacturing capabilities in Kaunas expanding.
Read More -
Hollister Incorporated Awarded SURPASS® Sole Source Contract for Enterostomal Therapy Products with Premier, Inc.
Need Help?
Whether you're a patient, a caregiver, or a healthcare professional, if you have any questions about Hollister products or services, we can help.
Prior to use, be sure to read the Instructions for Use for information regarding Intended Use, Contraindications, Warnings, Precautions, and Instructions.
The information provided herein is not medical advice and is not intended to substitute for the advice of your personal physician or other healthcare provider. This information should not be used to seek help in a medical emergency. If you experience a medical emergency, seek medical treatment in person immediately.
Welcome to Hollister Incorporated!
We want to make it as easy as possible for you to navigate our website. Please select your country and preferred language to ensure that you see customized content and accurate product availability information.